A student is often tempted to quickly move on to examination after listening to the presenting complaints.
Clinical history taking should not be taken lightly.
A logically taken history will give rise to a list of probable diagnoses in your mind by identifying patterns of symptoms even before you proceed on to the examination.
Systematically taken history will guide you to:
• Look especially for signs for confirming or ruling out certain disorders upon physical examination and
• Guide you to order the right investigations and to study the results of these investigations so as not to miss critical diagnostic clues.
History taking combines social skills with scientific knowledge. Therefore this skill constantly refines with increase in knowledge and experience.
For the beginners, it is important to follow some type of standard format for history taking so as not to miss important points that may help in clinching the correct diagnosis.
1. The first step in history taking is recording the socio-demographic data
• Name: may give a clue to the country/state of origin, religion etc. Each of these may increase or decrease the probability of certain diagnosis associated with the particular region or religion. E.g. chronic fever may be due to Kala-azar if the patient is from the endemic state
• Age: Probability of various disorders change with the age at presentation. E.g. congenital origin is more likely in young children, infections, vaccine preventable infections, nutritional deficiencies in older children and youth, degenerative and neoplasms probability rises in the elderly. A chronic cough may indicate COPD in middle age whereas the first possibility that comes to the mind would be carcinoma in case of a 65 yr. old
• Sex: Males are known to be more prone to disorders like Coronary heart disease, X-linked disorders, liver cirrhosis etc. On the other hand women are more prone to iron deficiency anemia, autoimmune disorders like hypo/hyper thyroidism, rheumatoid arthritis, SLE etc. Some diagnoses like BHP, ectopic pregnancy are possible in only one of the genders. One may need to rule out pregnancy for considering certain treatments.
• Religion: Religious practices like not smoking, not using alcohol, not eating meat etc. may increase or reduce the proneness to some diseases.
• Marital status: Similar complaints in the spouse increase the probability of some family practice as the reason behind the complaints. Certain anxiety disorders are associated with marital status. In addition, it may influence the plan of treatment.
• Address: some diseases may be more common in certain areas like falciparum malaria in North eastern states. In addition the address may indicate the socioeconomic status as that too affects the probability of certain diagnoses. For example, an urban residence raises the probability of stress related illnesses like IHD; DM, and HT. Fluorosis, goiter etc. is more likely in patients from endemic areas.
• Occupation: Certain occupations increase the risk of specific disorders like sedentary work is associated with cardio vascular diseases. Working in high temperatures e.g. in mines may affect the fertility in males etc. Occupation also gives information regarding the socioeconomic status of the patient.
• Source of history (Informant): who is the person giving you the information regarding the case? Usually, information provided by the patient himself is most reliable. In case of children, the mother’s information may be more reliable than that given by other relatives of the child.
2. The Presenting Complaint (aka ‘Chief Complaints’):
The Presenting complaint is the symptom for which the patient has reported to the health center/clinic.
Extremely important points while noting the presenting complaints are:
• It should be in the Patient’s OWN WORDS (NO directed questions)
• Record the individual symptoms in CHRONOLOGICAL ORDER of their appearance
• Among symptoms appearing at the same time, list them in order of severity as per the patient’s judgment.
It is noted as a list of symptoms, each followed by the duration For example:
1. Fever X 10 days
2. Cough X one week
3. Difficulty in breathing X 4 days
3. History of Presenting Complaint/illness:
Elaborate the chief complaints in detail. Ask for the sequential account of events from the onset of the symptoms to the present state. Allow him to elaborate (and record) in his own words. Be careful not to put any leading questions as these may divert the flow and twist the history leading to a wrong diagnosis.
The symptoms may be elaborated in terms of:
• Mode of onset: acute, sub-acute or gradual, any event preceding the onset etc.
• Symptoms Localized, diffuse or radiating
• Progression: increasing, decreasing, continuous or intermittent
• Aggravating and relieving factors
• Treatment taken and response to the treatment etc.
(The aspects to be asked regarding common presenting symptoms have been listed in another blog.)
Other associated symptoms: Elaborating the presenting complaints begins to suggest which system’s involvement and which pathology may explain the symptoms. Appropriate direct questions may be asked at this stage to rule out or confirm presence of these.
Enquire about presence of symptoms suggestive of disorders whose possibility comes to the mind. A negative answer here is as important as a positive one.
These questions are usually direct and need only a yes/no for an answer. This is sometimes referred to as taking the ‘negative history’. For example:
A patient with a presenting complaint of chest pain for last 3 months
Direct questions may be ‘does the pain start on physical exertion?’, ‘Does a period of rest relieve the pain?’, ‘Does the pain increase on coughing?’ and so on. A positive answer to the first two questions may suggest angina, whereas a negative answer will rule out the possibility.
Review of all systems:
For the sake of not missing any information, a review of all systems may be done by asking about symptoms pertaining to all systems. A table of such questions is given at the end of this blog
4. History of Past Illness:
The past medical history may provide valuable information about the current medical condition. In addition, it may provide information about the patient’s health seeking behavior and treatment compliance.
E.g. a past history of gonorrhea/urethral discharge may turn the diagnosis of arthritis to a possibility of gonococcal arthritis. A past history of similar headaches on one side may favor a diagnosis of cluster headache.
Care must be taken to counter check the past diagnoses as the patient may be using the medical terms loosely.
E.g. a chest pain patient may report a past history of angina. On further questioning, it may be found that the diagnosis was casually made by a non-medical friend and it seems that he had pulled a chest muscle while lifting heavy weight.
Ask:
• Similar illness in past
• Any illness that you think might be related to the current symptoms
• Any history of hospitalization
• Any history of surgery
• Any other illness
• History of chronic diseases like DM, HT, CHD, TB etc.
Example: a patient was operated for hernia and a mesh was placed by the surgeon. A past history of partially treated abdominal TB was missed. An active abdominal TB caused complications and the patient expired due to perforation peritonitis.
5. Treatment history
• Every effort should be made to obtain an accurate treatment history as it helps in following ways:
o Knowing the medication taken for the current illness and the response to this, can point towards the diagnosis or to the need of considering alternatives while planning the future treatment. The presenting complaint may be a side effect of the medicine or its interaction with another long term medication.
o Medicines may be masking some symptoms that you are expecting according to the differential diagnosis one has created in mind, while analyzing the history.
E.g. a person on beta blocker may not have the classic symptoms of hypoglycemia,
o To avoid duplication of prescription, interaction with current medication
• Obtain not only the list of prescribed drugs but also the patient’s compliance. Consider all drugs whether related or unrelated to the current complaints e.g. over the counter analgesics, oral/injectable contraceptives, psychotropic drugs etc.
• Also ask about other modes of treatment like surgeries, caesarian section etc.
• Enquire about any allergic or untoward reaction to any drug or treatment.
6. Family history
Ask the following:
• Family composition of the patient
• History of similar complaints in the family: may point towards a hereditary condition or a risk factor in the home environment of the patient
• Family history of the diseases which may be a part of the differential diagnoses in your mind: Many illnesses are associated with a positive family history and may increase the likelihood of the patient having the same illness. E.g. Breast cancer can be familial
• Any deaths in the family and causes for them
• Any history of hereditary disease in the family; history of consanguineous marriage in the family
• History of chronic disease in the family like HT, DM, TB etc.
• Any reason for stress in the family, e.g. Headaches in a school child may arise from anxiety from bullying at school
7. Occupational history
Occupational history is important for the following:
• Forming a diagnosis when there seems to be an occupational risk; e.g. infertility in a man may be due to exposure to consistently high temperatures while working in blast furnace factory, Cement, brick, glass factory. Sedentary occupation predisposes to lifestyle diseases
A suspected occupational link may clinch the diagnosis or causation; e.g. psittacosis pneumonia in those handling birds
• The patient may be unfit for the current occupation due to his condition and needs advice for change of occupation e.g. a patients with seizures must be cautioned against working a truck driver or deep sea diving.
• Certain protective measures can be advised in the current job for stopping the progression of the disease, e.g. a patient with CHD can request a work that does not involve strenuous physical activity.
• The occupation can indicate the socioeconomic status of the patient. This also has a bearing in forming the differential diagnoses
If the occupational history is incomplete, an occupational disease may remain undiagnosed or Job-related diseases may remain underdiagnosed or attributed to other causes.
An effort should be made to ask about the present and past occupations and the type of work executed at the job.
8. Dietary history
Assess the pattern of dietary intake:
Veg/non-veg (frequency of non-veg consumption in a week)/vegan
Amount of fruit and vegetables in daily intake
Any special diet due to any reason
Means of preparation of food like which oil/fat used, salt addition etc. if relevant
In suspicion of the disease being nutritional in origin e.g. iron deficiency anemia or thiamine deficiency in Neurologic symptoms, a detailed history may be taken. Estimating the daily intake of iron/thiamine may be useful
In special cases like an under 5 or pregnant female, 24-hour recall can be used to assess the calorie, protein and iron intake in the previous 24 hours. The findings may be presented as percent deficit of the daily recommendation
9. Personal history
History of smoking and number of cigarettes/beedies smoked in a day and the duration of smoking habit
History of using other forms of tobacco e.g. chewing tobacco (higher risk of oral cancer)
History of alcohol consumption
– Ever used alcohol
– Amount and frequency of alcohol consumption
Ask if the urinary and bowel habits are regular. Enquire about any recent change.
The living conditions may be assessed if any link with the present illness is suspected. Also in case of an elderly or dependent person, the management may depend upon this information; e.g. in an elderly lady with hip fracture it is important to know if she lives alone or relatives around her or if she has some other kind of support services or how suitable her house is for someone with reduced movement
10. Menstrual history
• Age of menarche
• Regularity of the cycles
• Duration of each cycle and number of days of bleeding
• Approximate volume of blood loss in each menstrual cycle
• Date of the Last menstrual period (L.M.P.): There may be a need to rule out pregnancy
If post- menopausal:
• Age of attainment of menopause
• Post-menopausal bleeding.
• Menopausal symptoms (ask also in peri-menopausal women)
11. Obstetric history:
• Number of pregnancies
• Number of deliveries, mode and place of deliveries
• Number of abortions, spontaneous and induced, reason if known
• Number of living children, their ages and the age of the last delivered child
• History of any antenatal problems (like eclampsia, edema feet, gestational diabetes), intra-natal and post natal complications
Additional categories are to be covered in special cases (Covered under specific blog/lecture)
Example: An under-5 child:
• Birth history: mode of delivery, indication for caesarian if any, history of delayed cry
• Feeding history: commencement of breast feeding, exclusive breast feeding, time of weaning etc.
• Immunization history: As per the current immunization schedule
• Developmental history: Assessment of age of attainment of developmental miles stones
Other examples of special cases are; a geriatric patient, psychiatric patient etc.
Making Sense out of Clinical History
You will be surprised to know that if properly taken, a diagnosis can be reached on the basis of the history alone.
Analyzing the history is similar to working of a detective. Identifying the pattern of symptoms, their evolution and associated symptoms indicates which organ system is involved.
Even though this analytical capability requires knowledge acquired through books and clinical experience, some principles can be understood at the starting itself. The type of pathology may be recognized.
Taking a meaningful history involves asking common-sense questions that can delineate the nature of a disorder and suggests the most likely pathophysiology, even if the diagnosis is not made at this stage. It does not take extensive and profound knowledge of medical facts.
For example:
• A rapid onset and progression over hours or days suggests infective or allergic pathology. You may ask questions to assess for localizing symptoms. A history of repeated episodes of similar symptoms may point towards an allergic/autoimmune phenomenon.
• A gradual onset with steady progression may point towards metabolic, malignant or a particular chronic disease. Associated symptoms of progressive weight loss, fatigue, old age etc. may point towards likely malignancy. Sudden onset with rapid progression may indicate vascular accident.
• The logic about which questions need to be asked to rule out or consider certain illness will grow as one continues to acquire understanding of pathophysiology of disease with time and knowledge.
• The detailed analysis can then be done by a senior and refined further on clinical examination and carefully chosen investigations.
Table for review of systems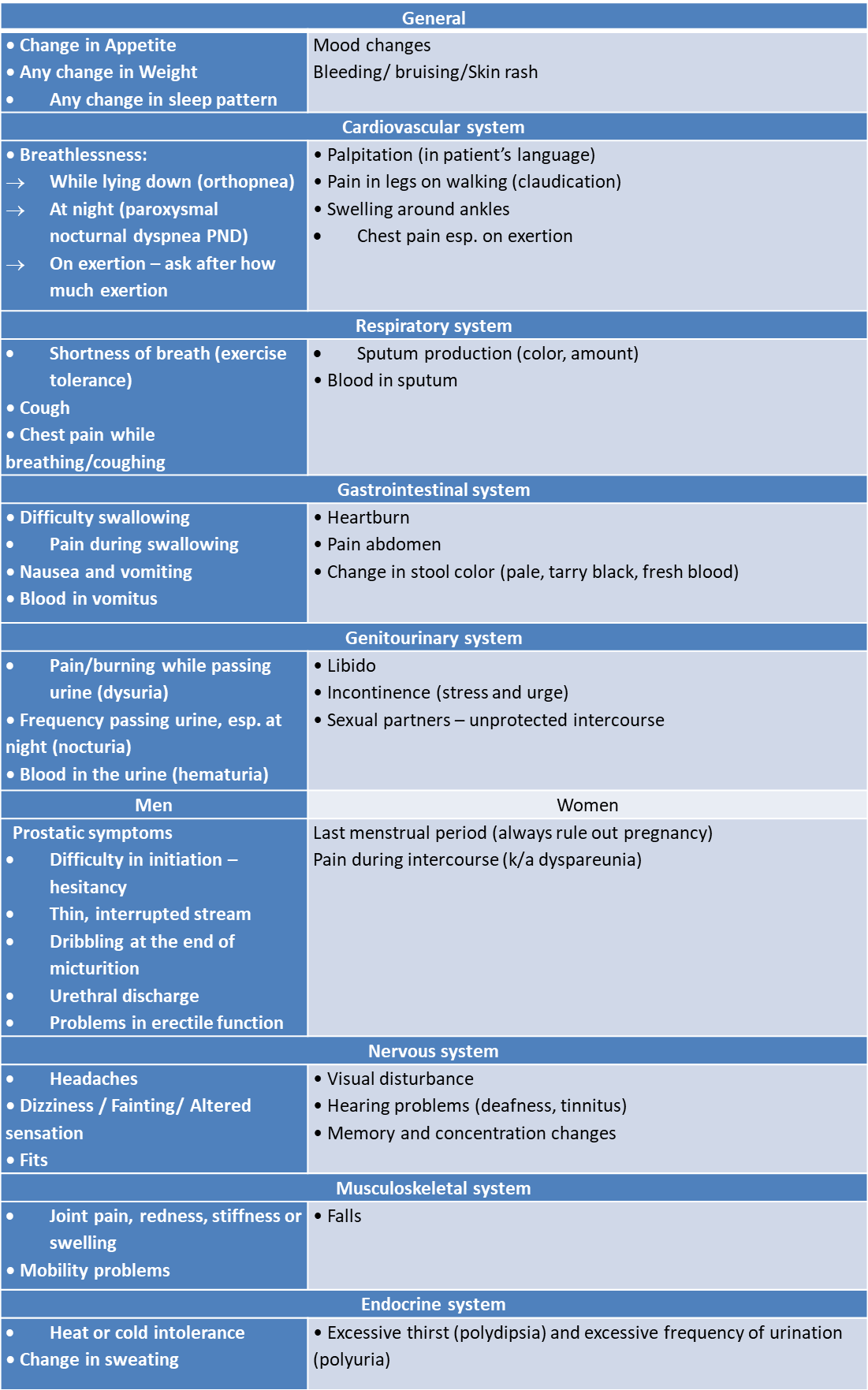
References:
1. R Alagappan. Manual of Practical Medicine. 4th ed. New Delhi. Jaypee Brothers Medical Publishers, 2011
2. Michael Glynn, William M. Drake. Doctor and patient: General principles of history taking .In HUTCHISON’S CLINICAL METHODS. 24th Ed. London. Elsevier, 2018: 20 – 31
3. Graham Douglas, Fiona Nicol, Colin Robertson. HISTORY TAKING AND GENERAL EXAMINATION. In Macleod’s Clinical Examination. 13th ed. Edinburgh. Churchil Livingstone Elsevier, 2013: 5 – 354
4. Hark L, Deen D, 1999. Taking a nutrition history: a practical approach for family physicians. Jr.Am Fam Physician. 1999 Mar 15;59(6):1521-8, 1531-2
5. Richard J. FitzGerald, 2009. Medication errors: the importance of an accurate drug history; Br J Clin Pharmacol; 67:6: 671–675
6. Driscoll CE. The Family History. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 215
7. UCSD's Practical Guide to Clinical Medicine; A comprehensive physical examination and clinical education site for medical students and other health care professionals. University of California, San Diego website. Available at: https://meded.ucsd.edu/clinicalmed/history.htm
4-Step Art of Diagnosis: What Medical School Can't Fully Teach: https://ihatepsm.com/blog/4-step-art-diagnosis-what-medical-school-cant-...
Introduction to history taking: https://ihatepsm.com/blog/introduction-history-taking-3rd-semester-students
Taking a Meaningful Clinical History: https://ihatepsm.com/blog/taking-meaningful-clinical-history
Format for Clinical History Taking: https://ihatepsm.com/blog/format-clinical-history-taking
History taking in a paediatric patient: https://ihatepsm.com/blog/history-taking-paediatric-patient
5-Page ANC History Taking Format: https://ihatepsm.com/blog/5-page-anc-history-taking-format-essential-gui...
Why ANC History Taking Matters?: https://ihatepsm.com/blog/why-anc-history-taking-matters
#Obstetric index (GPAL) in Antenatal Case History: https://ihatepsm.com/blog/obstetric-index-gpal-antenatal-case-history
#Decoding Gravida and Para: Terms in Antenatal History Taking: https://ihatepsm.com/blog/decoding-gravida-and-para-terms-antenatal-hist...
#Duration of Pregnancy: Understanding the Trimesters and Gestational Age Categories: https://ihatepsm.com/blog/duration-pregnancy-understanding-trimesters-an...
#Calculation of Expected Date of Delivery (EDD) and Period of Gestation (POG): https://ihatepsm.com/blog/calculation-expected-date-delivery-edd-and-per...
#Antenatal Care and Case Booking: https://ihatepsm.com/blog/antenatal-care-and-case-booking
#Clinical Significance of Antenatal History Components (Socio-Demographic components): https://ihatepsm.com/blog/clinical-significance-antenatal-history-compon...
Antenatal History Taking: Significance of Clinical Components: https://ihatepsm.com/blog/antenatal-history-taking-significance-clinical...
Trimester-wise History Taking in Antenatal Care: FIRST Trimester: https://ihatepsm.com/blog/trimester-wise-history-taking-antenatal-care-f...
Trimester-wise History Taking in Antenatal Care: SECOND Trimester: https://ihatepsm.com/blog/trimester-wise-history-taking-antenatal-care-s...
Trimester-wise History Taking in Antenatal Care: THIRD Trimester: https://ihatepsm.com/blog/trimester-wise-history-taking-antenatal-care-t...
Trimester-wise History Taking in Antenatal Care: A Comprehensive Guide (all 3 trimesters): https://ihatepsm.com/blog/trimester-wise-history-taking-antenatal-care-c...
Components of Birth Preparedness and Complication Readiness (BPCR): https://ihatepsm.com/blog/components-birth-preparedness-and-complication...
BPCR in brief: https://ihatepsm.com/blog/%E2%80%98birth-preparedness-and-complication-r...
Specific Health Protection during Antenatal Visits: https://ihatepsm.com/blog/specific-health-protection-during-antenatal-vi...
