Taking an antenatal history is not just about collecting facts. Every question in the history has a specific purpose, helping the clinician
• Assess maternal well-being
• Anticipate potential risks, and
• Plan appropriate care.
For students and young clinicians, it’s important to realize that every piece of information in the history has a clinical meaning. Knowing why a question is asked and what it indicates helps in interpreting the findings logically rather than memorizing them mechanically.
In this section, we will explore the significance of each component of antenatal history — explaining what it reveals, how it influences clinical decision-making, and why it is essential in ensuring safe and effective maternal care.
Name of the Patient
Accurate documentation of the patient’s name is essential for following purposes:
1. Identification: Ensures that all clinical notes, test results, and prescriptions are correctly matched with the patient, minimizing the risk of medical errors.
2. Communication and Rapport: Addressing the woman by name helps establish a respectful relationship and builds a good rapport which is vital for obtaining a reliable history.
Name of the Partner
Traditionally, the husband’s name was recorded to differentiate between women with similar names in hospital wards or registers. However, this convention is being reconsidered in the context of inclusive and non-discriminatory healthcare.
Consequently, using the term “partner” instead of “husband” and the prefix “Ms.” instead of “Mrs.” (unless the woman explicitly prefers otherwise) reflects inclusivity and gender sensitivity.
Demographic Profile and Its Clinical Significance in Antenatal History Taking
Basic demographic details—such as the woman’s age, residence, education, occupation, and socioeconomic background—play a crucial role in evaluating obstetric risk. These factors help clinicians identify women who may require additional surveillance or special management plans during pregnancy.
1. Importance of Age
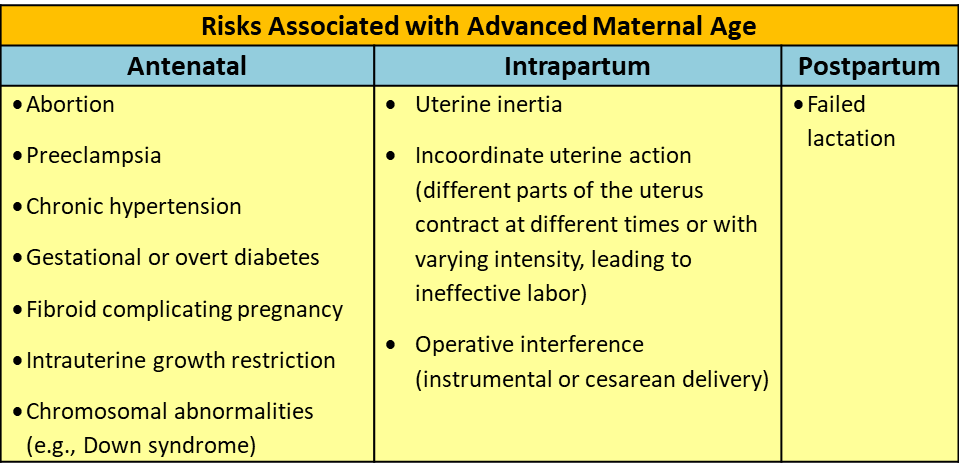
Maternal age significantly influences pregnancy outcomes. Obstetric complications are more frequent in teenage pregnancies (age ≤19 years) and in advanced maternal age (age > 35 years). Recognizing these risks helps tailor antenatal care and counseling.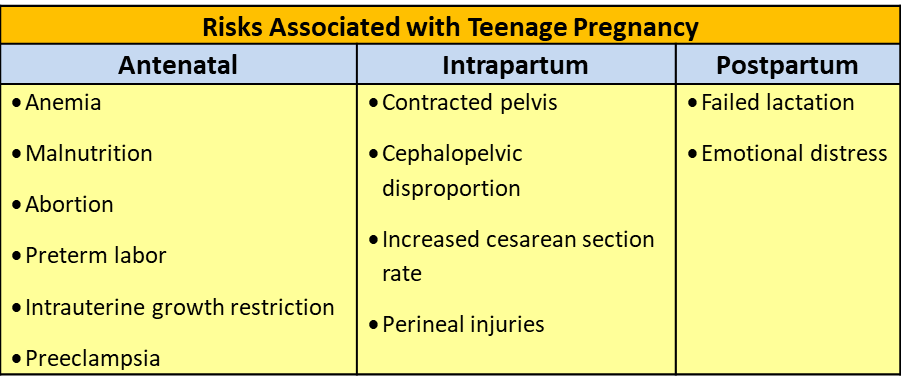
2. Importance of Residence
The woman’s place of residence is a key determinant in planning her care and ensuring safe delivery.
• Access to health services determines her ability to reach facilities, especially during obstetric emergencies.
o Women from remote areas may require admission at term, while those living near hospitals can be managed as outpatients in cases of mild preeclampsia, GDM etc.
o Certain regions are endemic for diseases such as filariasis, malaria, leprosy, and iodine deficiency disorders.
o Environmental and housing conditions also influence perinatal outcomes.
3. Importance of Education
Education improves awareness, compliance, and decision-making. Educated women are more likely to attend antenatal visits, follow dietary and drug advice, and participate in outpatient management for conditions like GDM or preeclampsia.
4. Importance of Occupation
There may be occupational risk factors. Some examples are given below: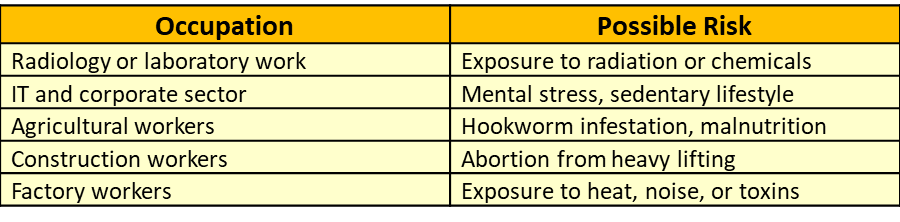
5. Importance of Socioeconomic Status (SES)
SES strongly influences maternal and perinatal outcomes. Lower SES is linked with infections, malnutrition, and anemia, while higher SES is associated with obesity, hypertension, and gestational diabetes.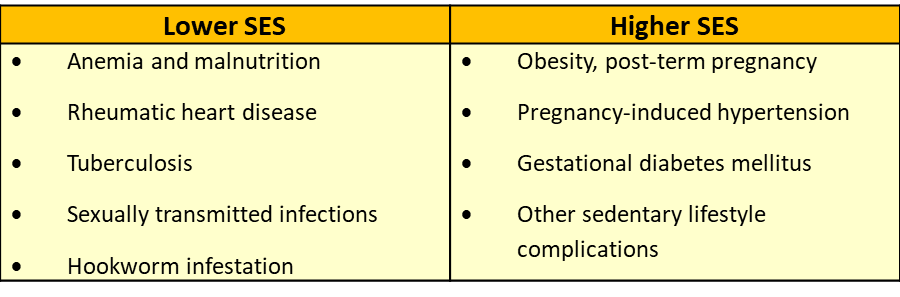
A patient’s socioeconomic status (SES) influences both dietary counseling and medication choices:
Dietary Advice: Recommendations should consider affordability.
• Women who can afford nutrient-rich foods may be advised to consume meat, liver, and egg yolk for anemia.
• For those with limited resources, equally nutritious but economical alternatives such as green leafy vegetables, jaggery, and ragi can be recommended.
Medication Prescriptions:
• Cost-effective options should be prioritized. Generic or lower-cost brands may be prescribed for patients who cannot afford expensive medications, ensuring adherence and continuity of care.
In India, the common scales for SES classification include Kuppuswamy’s Scale (urban), Modified BG Prasad Scale (urban & rural), and Uday Pareek Scale (rural). These are periodically updated to reflect inflation. (Ref: Sharma R, IJCM, 2024).
6. Importance of Nearest Health Facility
Knowledge of the nearest health facility helps in emergency preparedness and decision-making.
• It guides referral planning and helps determine if the patient can be managed on an outpatient basis or requires inpatient care. The proximity of a health facility plays a critical role in antenatal care and maternal outcomes:
o Emergency Access: Ensures timely care in obstetric emergencies such as hemorrhage, eclampsia, or obstructed labor.
o Management Decisions: Helps determine whether a patient can be managed on an outpatient basis or requires inpatient admission, depending on the severity of her condition and distance from the facility.
7. Importance of Period of Gestation (POG) and Expected Date of Delivery (EDD)
• Accurate knowledge of POG and EDD is fundamental in antenatal care:
o Guides diagnosis and risk assessment for conditions such as preterm labor, post-term pregnancy, and fetal growth restriction.
o Informs clinical decisions, including timing of investigations, interventions, and delivery planning.
Complications in a Primigravida
Women pregnant for the first time have an increased risk of certain obstetric complications, including:
• Preeclampsia
• Preterm labor
• Cephalopelvic disproportion (CPD)
Complications in a Grand Multigravida
Women with five or more previous viable pregnancies (grand multigravida) are at higher risk for antenatal, intrapartum, and postpartum complications: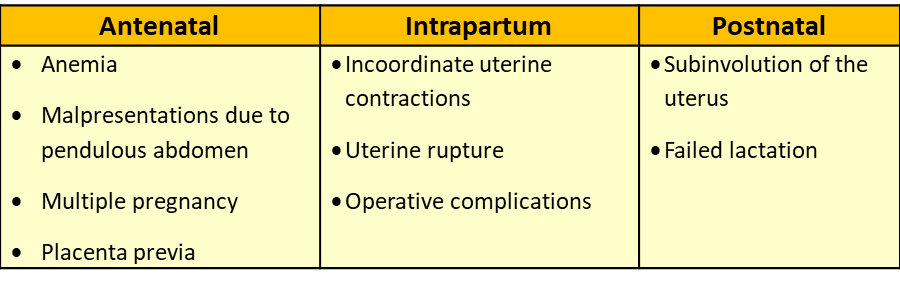
References
1. Ministry of Health and Family Welfare, Government of India. Guidelines for Antenatal Care and Skilled Attendance at Birth, 2010
2. Dutta DC. Textbook of Obstetrics. 9th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023.
3. Padubidri VG, Daftary SN. Shaw’s Textbook of Gynaecology. 18th ed. New Delhi: Elsevier; 2022.
4. Park K. Park’s Textbook of Preventive and Social Medicine. 28th ed. Jabalpur: Bhanot Publishers; 2025.
5. Babu SA. Clinical Obstetrics and Gynecology. 2nd ed. New Delhi: Wolters Kluwer India Pvt Ltd; 2025
5-Page ANC History Taking Format: https://ihatepsm.com/blog/5-page-anc-history-taking-format-essential-gui...
Why ANC History Taking Matters?: https://ihatepsm.com/blog/why-anc-history-taking-matters
#Obstetric index (GPAL) in Antenatal Case History: https://ihatepsm.com/blog/obstetric-index-gpal-antenatal-case-history
#Decoding Gravida and Para: Terms in Antenatal History Taking: https://ihatepsm.com/blog/decoding-gravida-and-para-terms-antenatal-hist...
#Duration of Pregnancy: Understanding the Trimesters and Gestational Age Categories: https://ihatepsm.com/blog/duration-pregnancy-understanding-trimesters-an...
#Calculation of Expected Date of Delivery (EDD) and Period of Gestation (POG): https://ihatepsm.com/blog/calculation-expected-date-delivery-edd-and-per...
#Antenatal Care and Case Booking: https://ihatepsm.com/blog/antenatal-care-and-case-booking
#Clinical Significance of Antenatal History Components (Socio-Demographic components): https://ihatepsm.com/blog/clinical-significance-antenatal-history-compon...
Antenatal History Taking: Significance of Clinical Components: https://ihatepsm.com/blog/antenatal-history-taking-significance-clinical...
Trimester-wise History Taking in Antenatal Care: FIRST Trimester: https://ihatepsm.com/blog/trimester-wise-history-taking-antenatal-care-f...
Trimester-wise History Taking in Antenatal Care: SECOND Trimester: https://ihatepsm.com/blog/trimester-wise-history-taking-antenatal-care-s...
Trimester-wise History Taking in Antenatal Care: THIRD Trimester: https://ihatepsm.com/blog/trimester-wise-history-taking-antenatal-care-t...
Trimester-wise History Taking in Antenatal Care: A Comprehensive Guide (all 3 trimesters): https://ihatepsm.com/blog/trimester-wise-history-taking-antenatal-care-c...
Components of Birth Preparedness and Complication Readiness (BPCR): https://ihatepsm.com/blog/components-birth-preparedness-and-complication...
BPCR in brief: https://ihatepsm.com/blog/%E2%80%98birth-preparedness-and-complication-r...
Specific Health Protection during Antenatal Visits: https://ihatepsm.com/blog/specific-health-protection-during-antenatal-vi...
