The aim of post–exposure prophylaxis is to neutralize the inoculated virus BEFORE it can enter the nervous system
• Every instance of human exposure should be treated as a medical emergency
• The components of prophylactic treatment are:
1. Local treatment of wound
2. Antibiotics and anti-tetanus measures
3. Active immunization against rabies – if indicated
4. Passive immunization with rabies immunoglobulin – if indicated
5. Observe the animal for 10 days from the day of bite:
• If healthy after 10 days: Discontinue post – exposure vaccination
• If dies within observation period: complete PEP
• If observation not possible: complete the post – exposure vaccination
Local Treatment of the Wound
• Prompt and adequate local treatment of all bite wounds and scratches is the first requisite
• The purpose of local treatment is to remove as much virus as possible from the site of inoculation before it can be absorbed on nerve endings
• Local treatment is of maximal value when applied immediately after exposure
1. If possible, within minutes
2. But it should not be neglected if several hours or days have elapsed
• Animal experiments have shown that local wound treatment can reduce the chances of developing rabies by up to 80%
Cleansing:
1. Immediate flushing and washing the wound/s, scratches and the adjoining area
2. With PLENTY of soap and running water (preferably under a running tap)
3. If soap is not available, at least simple flushing of the wounds with plenty of water should be done as first aid
4. In case of punctured wounds, catheters should be used to irrigate the wounds
Chemical treatment:
5. The residual virus after cleansing, should be inactivated by irrigation with virucidal agents
• Alcohol 400 – 700 ml/L or
• Iodine solution (tincture/ 0.01% aqueous solution/ povidone Iodine)
Avoid Suturing:
Bite wounds should NOT be immediately sutured
This is to prevent additional trauma as it may help spread the virus into deeper tissues
If necessary, it should be done 24 – 48 hr. later:
Applying minimum possible stitches
Under the cover of rabies immunoglobulin, LOCALLY
Local treatment is to be followed by:
• Antibiotic administration
• Tetanus toxoid if indicated
2. Immunization with rabies vaccine and immunoglobulin as per the table below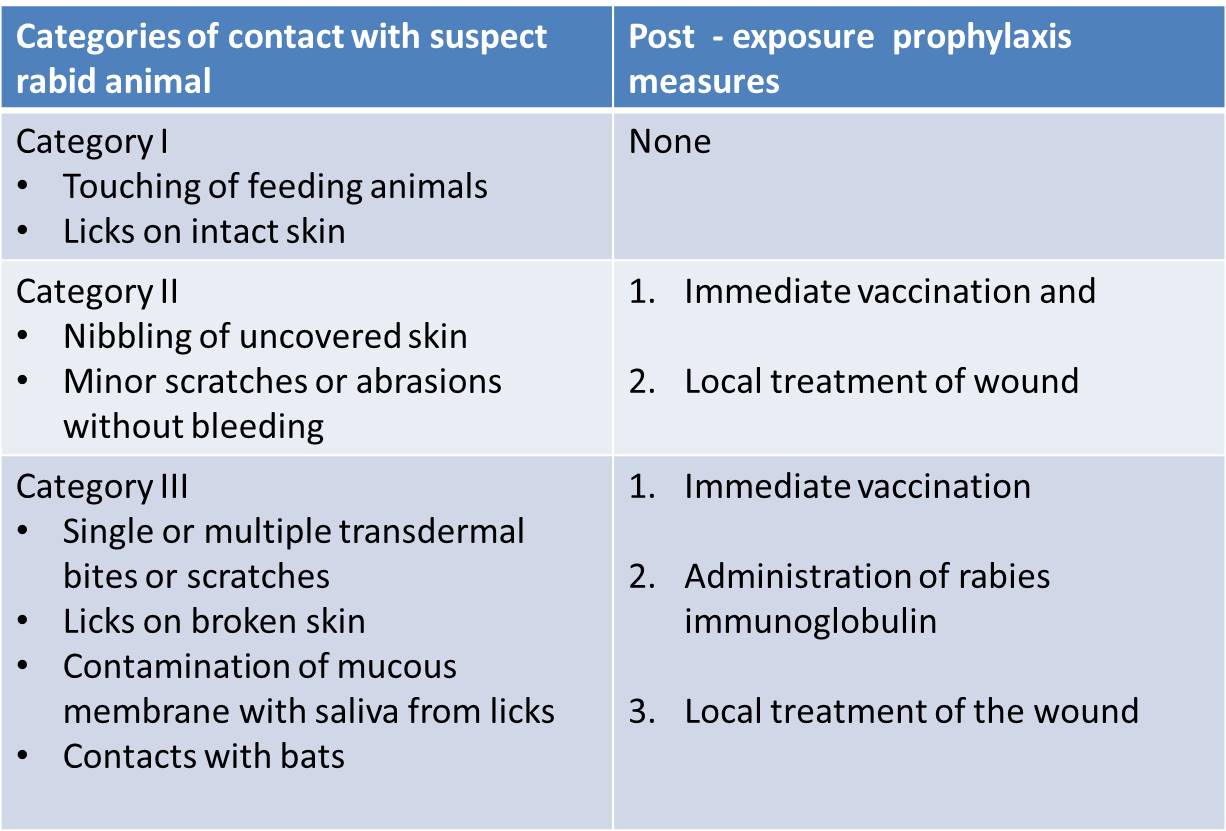
• Category II and III exposures carry a risk of developing rabies and require PEP
• This risk is higher if:
– The biting mammal is a known rabies reservoir or vector species
– The animal looks sick or has abnormal behavior
– A wound or mucous membrane was contaminated by the animal’s saliva
– The bite was unprovoked
– The animal has not been vaccinated and
– If the biting animal cannot be traced or identified
The vaccination status of the suspected animal alone should not be considered for deciding on PEP
• PEP may be discontinued/modified if:
– The suspected animal is confirmed to be free of rabies by laboratory examination or
– In the case of domestic dog/ cat, the animal remains healthy throughout the 10 day observation period starting from the date of the bite
However what is advised in the above scenario is:
•If Intradermal schedule is followed, complete the schedule
•If Intramuscular route is used, convert the schedule to that of the PRE exposure prophylaxis by omitting the day 14 dose.
This will be of help in future bites because;
•Lesser number of doses will be needed
•May eliminate the requirement for Rabies immunoglobulin
Reference:
Government of India, National rabies control programme, National guidelines on rabies prophylaxis, National Centre for Disease Control, 2019, Delhi, India.
Dog Bite: FAQs: http://www.ihatepsm.com/blog/dog-%E2%80%93-bite-frequently-asked-questio...
Post Exposure Prophylaxis (PEP) for rabies: http://www.ihatepsm.com/blog/post-%E2%80%93-exposure-prophylaxis-rabies
Rabies vaccine: http://www.ihatepsm.com/blog/rabies-vaccine
signs & symptoms of rabies in brief: http://www.ihatepsm.com/blog/signs-and-symptoms-rabies-brief
Categorization of animal bite: http://www.ihatepsm.com/blog/post-%E2%80%93-exposure-prophylaxis-rabies
Steps of immediate wound management in animal bite: http://www.ihatepsm.com/blog/steps-immediate-wound-management
Rabies Vaccination: http://www.ihatepsm.com/blog/rabies-vaccination
