1. NTP: National Tuberculosis Control Program, 1962
• Reviewed in 1992: NTP had not achieved its aims or targets
2. RNTCP: Revised National Tuberculosis Control Program, 1992
• Incorporating ‘Directly Observed Treatment Short-course’ (DOTS) strategy
Stop TB Strategy, 2006
Announced in 2006 by WHO and adopted by RNTCP
• Continue and expand DOTS
• Addressing TB/HIV
• Addressing MDR-TB
• Health system strengthening
• Engaging pvt and alternative practitioners
• Empowering patients
• Promoting research
– Diagnostics
– Treatment
– Vaccine
• National Airborne Infection Control Guidelines
• Practical Approach to Lung Health
End TB Strategy, 2014
• Approved by WHO in 2014, as TB was still the deadliest infectious disease globally
– A 20 year program
• Vision: Zero death, disease and suffering due to TB
• Interventions are both:
– Health related and
– Social (as TB is associated with social factors esp. poverty)
• End-TB Strategy includes
1. Patient centered care and prevention
2. Bold policies & patient support
3. Intensified research and innovation
3. NTEP: The program has been renamed as 'National Tuberculosis Elimination Program in 2020
• GOI (MoHFW )has committed to end TB by 2025,
– 5 years ahead of the global target under Sustainable Development Goals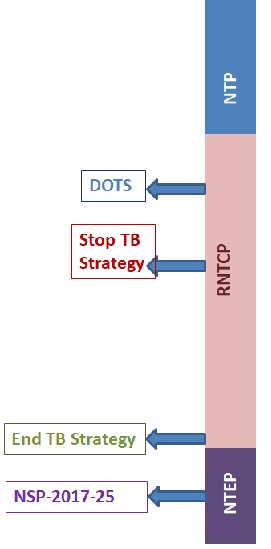
National Strategic Plan 2017-25 (NSP) has been made for Tuberculosis Elimination by 2025
• Major organizational change: creation of a sub-district administrative level i.e. at the Block/ PHC level
– The ‘Tuberculosis Unit’ (TU)
– MO-TC has the overall responsibility of management of TB Control Program at the TU
– The team of STS and STLS are under the administrative supervision of the MO-TC and the DTO
PHI is a health facility, having at least 1 medical officer.
• Dispensaries, PHCs, CHCs, referral hospitals, major hospitals, specialty clinics or hospitals, TB hospitals, ART Centres and Medical colleges in the district.
• Even the private and NGO participating in NTEP are considered as PHIs
• Some of these PHIs also function as DMCs.
• PHI has the main responsibility of case finding & management.
• If > 1 MO is posted in a PHI, one is to be identified for the responsibilities of the NTEP.
– Referral for screening for DM is the responsibility of the PHI where TB Rx is initiated
• All Diabetic TB patients should be linked for diabetic care.
TB Laboratory Services: 3-tier system
• The peripheral laboratories
• State level- Intermediate reference laboratory (IRL),
• Central level
For details, click here
Supporting Facilities for NTEP
NTEP: Key activities include
1. Active TB case finding
2. Newer and shorter regimen
3. Private sector engagement
4. Financial/nutritional support to TB patients
5. IT enabled
• surveillance,
• preventive and
• awareness measures
Active Case Finding (ACF)
Active case finding, as opposed to passive case finding, means:
Going out and identifying TB in individuals who don’t come themselves for health care using community volunteers with proper training and supervision
• ACF is to be done in among high-risk groups (HRGs) Which have been identified as:
1. PLHIV (people living with HIV)
2. All contacts of bacteriologically confirmed pulmonary TB patient
3. Other risk groups (silicosis, immuno-compromised, organ transplant, hemodialysis, anti TNF-therapy, etc).
4. Migrants
5. People living in
– urban slums,
– construction sites, and
– hard-to-reach areas
• It’s planned to conduct 3 rounds of ACF/year
• TB patients detected during ACF are referred for Dx and TB Rx
• Patients with other morbidities
TB Comorbidities
(Detecting TB in patients with other Morbidities)
TB and HIV
• HIV Testing for TB Patients (including Presumptive TB cases)
• Screening for TB among HIV patients (Intensive Case Finding /ICF)
– using 4 symptom complex
1. Cough of any duration,
2. Fever,
3. Weight loss,
4. Night sweat
• ICF is to be done at ICTC, ART center and Link ART Centers
– ICF is also to be done even among HIV high risk groups (HRG)
– Isoniazid preventive treatment (IPT) for all people living with HIV (PLHIV)
– TB pt. with HIV: same daily treatment for same duration as HIV-negative TB pts.
TB and Diabetes
• Screening of TB patients for Diabetes
– If DM found, then linkage to DM care center
• Screening of Diabetes patients for TB (4 symptom complex/every visit)
– If found to have TB, linkage with TB management center
Newer & Shorter Regimens
For details, click here
Patient support for TB Elimination
1. Treatment Support
2. Adherence support strategy
3. Nutritional Support
4. Mitigating catastrophic expenditure (such as those provided through DBT)
5. Airborne infection control in Community and Facility
6. Patient help desk and grievance redressal.
Treatment & Adherence Support
1. To Minimize delay in starting treatment
2. Maximize adherence by
– Monitoring & reporting dose administration
– Support for preventing treatment interruption
A support plan is developed right at time of diagnosis, in consultation with the patient and the relevant health staff.
This plan should include:
1. A home visit for counseling of the patient and family members
2. Follow-up schedule at PHI and for lab investigations
3. Linkages for co-morbidity management
– including assessment of nutritional status and nutrition support
4. Adherence support using tools like
– 99DOTS,
– Retrieval of treatment interrupters,
– Screening for adverse reactions,
– Supervision of treatment supporter etc.
Nutritional support
• All individuals with active TB receive
(i) An assessment of their nutritional status and
(ii) Counseling based on their nutritional status
– At diagnosis and throughout their treatment.
(iii) Any malnutrition detected, is managed as per WHO recommendations.
• NTEP guidelines for nutritional assessment and counseling of TB patients are in the Document
– Nutritional Care & Support for TB patients in India
Nikshay Poshan Yojana (NPY)
• DBT at notification and then during treatment
(DBT=Direct Benefit Transfer i.e. money credited directly to the beneficiary’s account)
– Rs. 500 each month of treatment and
– Up to Rs. 1000 as an advance.
Mitigating catastrophic expenditure
• Catastrophic expenditure: Includes expenses for tests, medicines, travel, loss of wages etc.
• An END TB Goal is: reducing catastrophic expenditure
1. Free diagnostic and treatment for the private sector too
2. Financial support to patients and care providers (DBT)
a. Nutritional Support (Rs.500/-month)
b. Travel support to Tribal Patients (Rs750/-)
c. Private Practitioners incentives (Rs.500/- for Notification & Rs.500/- for reporting of Treatment Outcome )
d. Treatment supporters Honorarium (Rs.1000/- to Rs.5000/-)
Support for airborne infection control
• TB patients are educated on prevention of airborne infection
– At home and at work place.
– E.g. cough hygiene
• Airborne infection control measures are implemented in Health Facilities, Community, and at household level.
• Health facilities
– Increased ventilation,
– Reduced crowding,
– Faster processing of patients’ and samples (fast tracking),
– Wet mopping
– Cough etiquette
• Patients are provided with
– Spittoon
– Disinfectant and
– Reusable masks and educated on their use.
• During house visits, the health workers observe for cough hygiene and reinforce AIC information.
• Details can be found the ‘Guidelines for Airborne infection control’.
Patient Grievance Redressal
• Patients can provide feedback and report grievances to the DTO on
– Paper or email or
– Through the National Call Centre (Nikshay – Sampark).
• If the request/grievance is not addressed at a particular level it will be escalated to the next higher level.
• At all points, the patient should be informed of the status of his/her submission
Supporting TB Patients under Private Providers
• TB control officers mustn’t attempt to divert patients from private providers to the public system
– Regulatory measures must also be used judiciously.
• The approach includes:
– Engagement of providers
– Linkage of services
– Patient support/ Public health actions
– Regulatory Measures
– Process of engagement of PPs
• 1. Engagement of providers
1. Mapping of private providers-
• Allopathy and AYUSH
• Chemists
• Laboratories
• NGO, corporate sector, health facilities under other Ministries, Public Sector Enterprises etc.
2. Prioritization of providers by DTO
• Following is considered for prioritization
1. allopathic practice
2. Patient load (Respiratory or TB patient load)
3. AYUSH providers
4. Pharmacies and their TB prescription load.
5. Diagnostic laboratories with TB diagnostic services and their test load
3. Collaborate with Private Providers
• All providers should be registered in NIKSHAY
• DTO can involve an NGO/agency to reach out to private providers.
• The private providers are sensitized through
1. Clinic visits, peer pressure or professional associations
2. Scientific and clinical information about TB management
• Then an onboarding kit is provided to the doctor
1. Notification formats
2. List of diagnostic/treatment services free & paid
• E.g. free X-ray, smear microscopy, CBNAAT, TrueNat etc.
3. Free anti-TB drugs
4. Sputum collection containers/falcon tubes 

Regulatory measures
1. GOI has made notification of TB cases mandatory on 7th May 2012.
– Legal backing for not notifying a TB patient.
– punitive measures as per IPC 269 & IPC 270.
– Use clinical establishment act (CEA) wherever it is being implemented.
– This will help to identify providers who are registered under the CEA and not registered with NIKSHAY
Involvement of Medical colleges in NTEP
• Facilities like
– DMC/CBNAAT lab,
– Treatment centre,
– Drug resistant TB centre etc. in Medical Colleges.
• It also facilitates research pertaining to TB in Medical colleges.
• Core Committees in medical colleges for inter-departmental coordination
– Operational research is one of the important activities of Medical Colleges.
Treatment of Pediatric TB
• For pediatric patients, formulations with daily dosages as per 6 weight band categories are made available
– All adolescents up to 18 years of age and weighing less than 39 kg, are to be treated using pediatric weight bands and
– Children weighing more than 39 kg with adult weight bands
IPT (isoniazid preventive treatment) in children:
• Preventive chemotherapy with isoniazid (H)
• All children ≤ 5 years who are in contact with all forms of Drug sensitive TB case.
– They are examined and investigated to rule out active TB
– If found to have TB, they are treated appropriately
– If active TB is ruled out, IPT given
• IPT dosage: INH 10 mg/kg body weight daily for 6 months.
TB in the Private Sector
• Standards for TB care in India: Guidelines made available for treatment & follow-up of TB patients
• Mandatory TB notification
• NIKSHAY: a web enabled application to facilitate monitoring of universal access to TB patients data by all concerned
• Ban on Sero-diagnostics and
• Regulatory tools are limited.
National Strategic Plan 2017-25
NSP has 4 pillars of strategy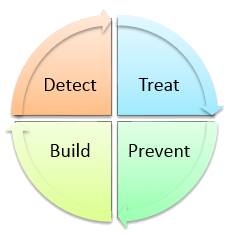
1. Detect: all drug sensitive cases (DS-TB) and drug resistant TB cases (DRTB) esp. from pvt providers and undiagnosed TB cases in high-risk groups (prisoners, migrant workers, PLHIV/AIDS, contacts etc.).
– And report these
2. Treat: Provision of free TB drugs in the form of daily fixed dose combinations (FDCs) for all TB cases is advised with the support of directly observed treatment (DOT).
– Screening of all patients for rifampicin resistance
3. Prevent
– Air-borne infection control measures at health care facilities
– Treatment for latent TB infection in contacts of bacteriologically-confirmed cases
– IPT
– BCG
– Address social determinants of TB through intersectoral approach.
4. Build: Health system strengthening for TB control
– enabling policies, empowering institutions and human resources
References
• Park’s Textbook of Preventive & Social Medicine, 26th ed. 2021. Bhanot Publishers, Jabalpur, M.P., India
• TRAINING MODULES (1-4) FOR PROGRAMME MANAGERS AND MEDICAL OFFICERS; New Delhi, India: Central TB Division, MoHFW, Government of India; July 2020., Available from:www.tbcindia.gov.in
• Prathiksha G, Daniel BD, Natrajan M. Active case-finding for tuberculosis in India. Natl Med J India 2019;32:90-95
