Introduction:
• Three major clinical types
– Anterior nasal
– Faucial and
– Laryngeal
• Rarely, other body parts may be affected
– Skin
– Conjunctiva
– Vulva etc.
• The bacilli multiply locally (mostly this site is the throat) and elaborate a powerful exotoxin which causes the following:
1. Formation of a greyish or yellowish membrane commonly over the
• tonsils,
• pharynx or
• Larynx or
• At the site of implantation
– This is a false membrane with
• Well defined edges and
• Cannot be wiped away
2. Marked congestion, edema or local tissue destruction
3. Enlargement of regional lymph nodes
4. Signs and symptoms of toxemia
• Average Fatality rate is about 10% in untreated cases
• Fatality rate in under 5 yr. children is 20% of untreated cases
Problem Statement
• World
• Rare disease in the developed countries
• Reason is routine vaccination of children
• Countries with satisfactory vaccination schemes,
• the disease has declined to a level that it is no longer a PHP
• A case may occasionally be seen among the non immunized children in developed countries
• Natural immunity against diphtheria is acquired by frequent skin infection with C. diphtheriae
• Improved SE conditions have changed this situation in developed world leading to a change in epidemiology of diphtheria
• Some outbreaks have demonstrated a shift in the age distribution of cases to older children and adults
• In developing countries
• The disease is endemic due to lack of widespread immunization
• India
• Diphtheria is endemic
• Declining trend, due to increasing immunization coverage
• CFR of about 2.6%
Agent Factors
• Agent is C diphtheriae
• Gram positive
• Non motile bacilli
– No invasive power
– Produces a powerful exotoxin
– Four types of bacilli, all are pathogenic to man
• Gravis
• Mitis
• Belfanti and
• Intermedius
• In general, gravis infections tend to be more severe than mitis infection
– All strains are not toxigenic
• Evidence suggests that non–toxicogenic strain can convert to toxicogenic upon exposure to the beta – phage (a bacteriophage)
– The toxin can affect
• The heart, leading to myocarditis or
• The nerves, leading to paralysis
• Sensitivity:
– Sensitive to Penicillin
– Sensitive to
• Heat and
• chemical agents
– They survive for short periods in dust and fomites
Source of infection
• Case or
– Range from subclinical to frank clinical
– Mild to moderate cases may present as only running nose or sore throat
– These play more important role than frank cases in the spread of infection
• Carrier
– Common source of infection; Carrier: cases = 95: 5
– Carrier may be
• Temporary or chronic
• Nasal or throat
– Nasal carriers are shed more frequently and hence more dangerous as source
– Temporary, carrier state may last about a month; chronic carrier state may persist about a year, unless treated
– Incidence of carriers in a community varies 0.1 – 5%
– Immunization does not prevent carrier state
Infective material
– Nasopharyngeal secretions
– Discharge from skin lesions
– Contaminated fomites and
– Possibly infected dust
Period of infectivity
– Unless treated, lasts from 14 days to 28 days from the onset of the disease
– Carriers remain infective for much longer periods
– A case or carrier is considered non – communicable:
Host Factors
Age
• Affects particularly children aged 1 yr. to 5 yr.
• In countries with widespread immunization, a shift in age incidence has been observed from preschool to school age
Sex:
• Both sexes are affected
Immunity
• Infants born of immune mothers are relatively immune during first few weeks or months of life
• Before artificial immunization,
– large proportion of population in developing countries were acquiring active immunity through in - apparent infection resulting in widespread production of antitoxin in the population
– Thus most members of the population except children were immune
– By age 6-8 yr. appx 75% of children in developing countries where skin infection with C are common, have protective serum antitoxin levels
• Diphtheria is principally the result of action of the toxin formed by the organism rather than invasion by the organism,
– resistance to the disease depends largely on the availability of specific neutralizing antitoxin in the bloodstream and tissues
• Diphtheria occurs only in persons who possess no antitoxin
Environmental factors
• Cases occur all seasons
• Winter months favor its spread
Mode of transmission
• Mainly by droplet infection
• Can also be transmitted directly to susceptible persons from infected cutaneous lesions
• Transmission by contaminated objects like cups, thermometers, toys, pencils is possible but only for short periods
Portal of entry:
• Respiratory route
– Commonly the portal of entry
• Non – respiratory route:
– Skin: cuts, wounds and ulcers may get infected
– Umbilicus in the newborn
– Occasional ports of entry
• Eye
• Genitalia or
• Middle ear
– Less common in developed countries, here spread by droplet infection is more common
Clinical Features
• IP: 2 to 6 days, occasionally longer
• Respiratory tract forms:
– Pharygotonsillar
– Laryngotracheal
– Nasal and
– Combinations
Pharyngotonsillar diphtheria
• Sore throat, difficulty in swallowing and low grade fever
O/E:
• Mild erythema throat
• Localized exudate or pseudo-membrane
– On posterior wall of pharynx or on tonsil
– May cover entire tonsil or less frequently even the soft and hard palates
– Pseudo membrane may be whitish and wipe off easily in early stage
– Later the membrane may become thick, blue-white to grey-black and adherent
– Attempts to remove the membrane result in bleeding
– A minimal area of mucosal erythema surrounds the membrane
• In severe disease
– Marked edema of submandibular area and anterior neck and
– Lymphadenopathy giving a characteristic ‘bull necked appearance
Laryngotracheal diphtheria
• Often preceded by pharyngotonsillar disease
– Fever
– Hoarseness
– Croupy cough
– If infection extends into bronchial tree, it is the most severe form of disease
– Initially the may be indistinguishable from viral croup or epiglottitis
– Prostration and dyspnea soon follow because of the obstruction by the membrane
– This obstruction may even cause suffocation if not promptly relieved by intubation or tracheostomy
Nasal Diphtheria
• Mildest form
• Localized to the septum or turbinates of one side of the nose
• Occasionally the membrane may extend into the pharynx
Cutaneous diphtheria
– Common in tropical area
– Often appears as a secondary infection of a previous skin abrasion
– Presenting lesion is often an ulcer
– Ulcer is
• Surrounded by erythema
• Covered with a membrane
– Patients generally seek treatment because of the chronicity of the skin lesion
– The bacilli within the membrane continue to produce toxin actively
– This is absorbed and results in distant toxic damage, particularly
– parenchymatous degeneration, Fatty infiltration and necrosis in
• Heart muscle
• Liver
• Kidneys and
• Adrenals
– Irregularities in cardiac rhythm indicate damage to the heart
– Later there may be difficulties with
– Vision
– Speech
– Swallowing or
– Movement of the arms or legs
– The toxin also produced nerve damage, leading to paralysis of the
– Soft palate
– Eye muscles or
– Extremities
– Those who survive these complications, recover completely
Control of Diphtheria
1. Treatment of
– Cases and
– Carriers
– Management of the ‘Contacts’ and
3. At the community level
– Increasing coverage of immunization with diphtheria toxoid
Treatment of Cases and Carriers
Early detection
• An active search for cases and carriers should start immediately amongst family and school contacts
• Carriers can be detected ONLY by culture
• Swabs should be taken from both the nose and throat
• Examined by culture for diphtheria bacilli
• Tests should also be done for virulence of the organism
Isolation
• All cases
• Suspected cases and
• Carriers should be
• Promptly isolated
• Preferably in a hospital
• For at least 14 days or
• Until proved free of infection
• At least 2 consecutive
• nose and throat swabs,
• taken 24 hours apart
• should be negative before terminating isolation
Treatment of cases and carriers
• Cases:
– Diphtheria antitoxin should be given without delay,
• IM or IV, Dose ranges from 20,000 to 1,00.000 units depending up on the severity
• Mild early pharyngeal or laryngeal disease: 20 to 40,000 units
• Moderate nasopharyngeal disease : 40 to 60, 000 units
• For severe, extensive or late (≥3 days): 80 to 1,00,000 units
– Penicillin or erythromycin for 5 – 6 days to clear the throat of C. diphtheriae and thereby decrease toxin production
– The case should be reported to the health authorities Immediately
– Once recovered, active immunization with diphtheria toxoid should be provided
• Carriers:
– Treat with 10 days course of oral erythromycin
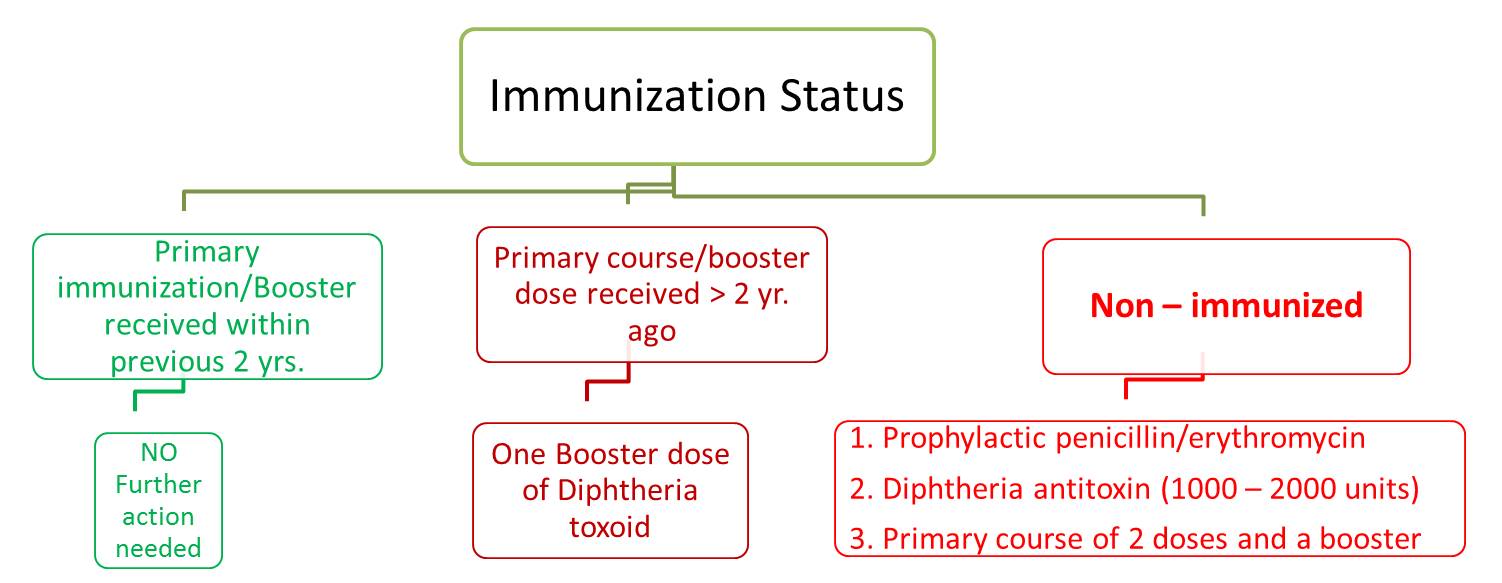
Management of Contacts
Contacts merit special attention
1. They should be throat swabbed
2. Determine the immunization status and take further action accordingly (shown below)
3. Contacts need to be placed under medical surveillance
– Examined daily for evidence of diphtheria for one week
– Bacteriological surveillance weekly for several weeks (weekly swabbing)
References
• DIPHTHERIA - A RE-EMERGING THREAT. CD Alert, Jan – Mar 2008; 12 (1): 1-8 available on http://www.ncdc.gov.in/writereaddata/linkimages/Jan-March%20087398246488... downloaded on 16 Dec 2016
• Communicable Disease Management Protocol – Diphtheria. August 2016. available at: http://www.gov.mb.ca/health/publichealth/cdc/protocol/diphtheria.pdf downloaded on 16 Dec 2016
• http://www.immunize.org/catg.d/p4203.pdf accessed on 16 Dec 2016
• Park’s Textbook of Preventive and Social Medicine, 23rd Edition, Diphtheria, 161-163
(adsbygoogle = window.adsbygoogle || []).push({
google_ad_client: "ca-pub-2296304216845141",
enable_page_level_ads: true
});
Control of diphtheria: http://www.ihatepsm.com/blog/control-diphtheria
Management of Contacts of a Case of Diphtheria: http://www.ihatepsm.com/blog/management-contacts-diphtheria-case
Diphtheria – Epidemiology, Clinical Features & Management: http://www.ihatepsm.com/blog/diphtheria-%E2%80%93-epidemiology-clinical-...
