Tetanus is a dangerous infectious disease characterized by muscle spasms. It is caused by the toxins (potent neurotoxin) secreted by a bacterium k/a Clostridium tetani.
Tetanus may occur at any age and case-fatality rates are high even with intensive care. Without medical care, the case-fatality rate is almost 100%.
The bacteria survive as spores in soil. These spores are ubiquitous around the world and may remain infectious for very long time; more than 40 years.
Once the spores gain entry into the body through a breach in the skin caused by any injury (or through the umbilical cord stump in the neonate), they germinate under anaerobic conditions.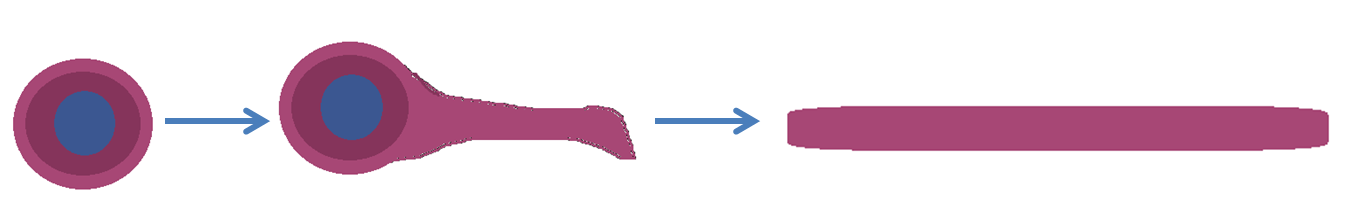
Active bacteria formed by germination of spores, multiply locally in the anaerobic conditions provided by the deep wound, debris in the wound etc.
These bacteria secrete a very potent toxin (Tetanospasmin) which enters the blood and reaches the central nervous system (CNS).
The toxin bound to CNS causes the typical signs and symptoms of tetanus which has a high mortality.
The risk of developing tetanus after an injury depends upon the following:
1. Type of the wound: i.e.
• How prone is the wound to development of tetanus?
• If anaerobic conditions are provided.
• Superficial/deep/puncture wound/sharp cut/crush injury/open fracture etc.
2. Condition of the wound: If high risk of contamination by C. tetani spores.
• Clean/contaminated with soil, feces, saliva, animal feces etc. / wounds containing debris and necrotic tissue/ presence of foreign body etc.
3. Immune status of the patient: If patient’s blood contain antibodies in sufficient amounts to neutralize any toxin absorbed from the wound.
• Complete primary immunization with 3 doses/ booster received;
• If yes, how long back etc.
Hence the aim of tetanus prophylaxis following injury is:
1. Timely removal of C. tetani from the wound/s before they can produce critical amounts of toxin
2. Deactivate any toxin that be already absorbed from the wound/s before it can reach the CNS
Therefore management of physical injury consists of:
1. Appropriate debridement and cleaning of the wound, if needed, to remove anaerobic conditions
2. Administering Tetanus Immunoglobulin (TIG)
• if high risk of tetanus is considered
3. Age & immune status appropriate dose/s of Tetanus toxoid containing vaccine
Following flow-chart provides a systematic assessment of the type and condition of wound plus immune status of the patient and suggests the appropriate management: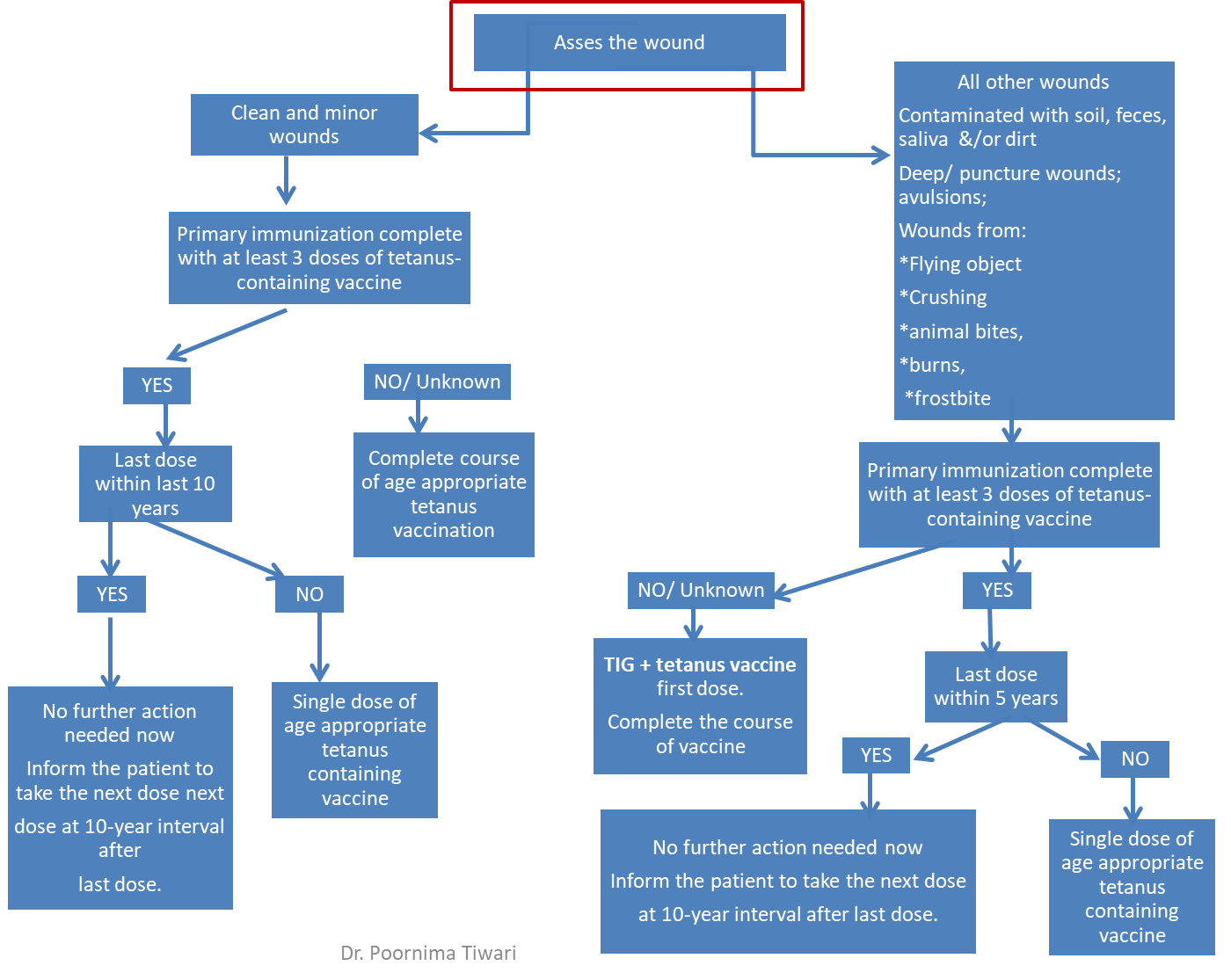
An age appropriate tetanus containing vaccine is to be used viz. DPT, TDaP, DT, TT or Td.
The most commonly used tetanus vaccine following injury, after 5 years of age has been Tetanus Toxoid (TT) till recently.
Government of India, since 2018, has started replacing of TT vaccine with Td vaccine in a phased manner for all age groups, including pregnant women.
This step is in consideration of increasing numbers of cases of diphtheria in older age groups in India and other countries.
Reference:
• Park K. Epidemiology of Communicable Diseases. In: Park's Textbook of Preventive and Social Medicine, 26th ed. Jabalpur, India: M/S Banarasidas Bhanot Publishers; 2021
• Summary Guide to Tetanus Prophylaxis in Routine Wound Management. Available at: https://www.health.state.mn.us/diseases/tetanus/hcp/tetwdmgmtc.pdf, accessed 16th April 2022 at 1:00 PM
• Government of India, MoHFW; Tetanus and adult Diphtheria (Td) vaccine; Operational Guidelines available at: https://nhm.gov.in/New_Updates_2018/NHM_Components/Immunization/Guildeli... downloaded on 16th April 2022 at 1:00 PM
