
IMNCI — Integrated Management of Neonatal and Childhood Illness (India)
Summary: IMNCI is India's adaptation of the WHO/UNICEF Integrated Management of Childhood Illness (IMCI) program. It emphasizes syndromic, evidence-based case management for children under five and adds focused modules on the neonatal period to address a major portion of infant deaths.
Major causes of infant & child mortality in developing countries
- Acute respiratory infections
- Diarrhoea
- Malaria
- Measles
- Malnutrition
Why single diagnoses are sometimes not feasible
- Children often present with overlapping signs and symptoms of multiple diseases.
- Clinical outcomes depend on treating both presenting symptoms and underlying disorders.
- At first-level health facilities, diagnostic tools (laboratory tests, X-ray) may be limited or absent.
Care-seeking behaviour & quality gaps
Every day millions of parents seek care from health centres, pharmacists, doctors, hospitals and traditional healers. Surveys show many sick children are not properly assessed or treated, and caregivers frequently receive poor advice. Limited diagnostics, drugs and equipment at peripheral facilities make quality care a serious challenge.
IMCI → IMNCI: the Indian adaptation
Integrated Management of Neonatal and Childhood Illness (IMNCI) was adapted for India to specifically address neonatal mortality (which constitutes a large share of infant deaths) and high early-infant mortality during the first two months of life.
Why India adapted IMCI to IMNCI
- Neonatal mortality contributes to a large portion of infant deaths; many deaths occur in the first week of life.
- Mortality in the second month of life is also higher than later ages.
- Any program aiming to reduce infant mortality must address the first two months, especially the first week.
- IMNCI targets children < 5 years but gives additional focus to neonates and young infants (0–2 months).
How IMNCI differs from IMCI
- Includes the 0–7 day age group explicitly.
- Training begins with sick young infants up to 2 months (in IMCI this occurs after training for 2 months–5 years).
- Training time for sick young infants and for the 2 month–5 year age group is roughly equal.
- Skill-based approach that incorporates national guidelines on malaria, anaemia, vitamin A supplementation and immunization.
Basis of IMNCI guidelines
The IMNCI clinical guidelines target children under 5 and use a syndromic, evidence-based approach to support rational, effective and affordable use of drugs and diagnostic tools.
- Evidence-based medicine: uses clinical research and cautions against relying on untested intuition.
- Syndromic approach: suitable where lab support is limited; careful assessment of symptoms and selected signs guides effective action.
- This approach helps the health worker determine: the likely health problem(s), severity, and appropriate actions (refer, manage in clinic, or advise home care).
The integrated case-management process
The process is presented as a series of charts that guide the health worker step-by-step:
- Assess the young infant or child — history + physical exam.
- Classify the illness — decide severity and assign a colour-coded classification (not a specific disease diagnosis).
- Identify treatment — the chart recommends treatment for each classification.
- Treat — give treatment in clinic, prescribe drugs or home treatments, and teach the caregiver.
- Counsel the mother/caregiver — feeding, fluids, danger signs and when to return.
- Give follow-up care — plan timely follow-up and referrals if needed.
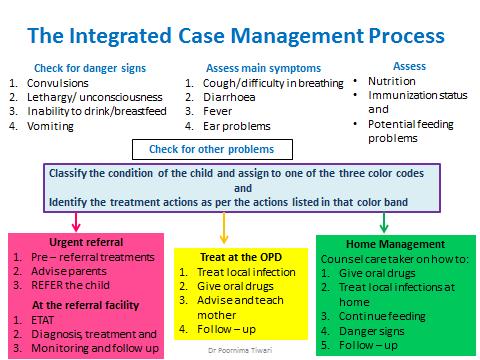
IMNCI case-management process (display charts prominently at the facility).
IMNCI wall charts and where to display them
The charts are designed for easy, quick decision-making and should be displayed prominently. Two main sets:
- Young infant (up to 2 months) — two charts:
- Assess & classify the sick young infant (up to 2 months)
- Treat the young infant and counsel the mother
- Child (2 months–5 years) — three charts:
- Assess & classify the sick child (2 months–5 years)
- Treat the child
- Counsel the mother
The three components of the IMNCI strategy
- Improve case-management skills of health staff through IMNCI guidelines (frontline worker training).
- Strengthen the overall health system required for effective management of childhood illness (supply chain, supervision, referral systems).
- Improve family & community practices and involve them in prevention, care-seeking and follow-up.
Other IMNCI training adaptations
- Pre-service IMNCI: being integrated into medical college curricula to create trained manpower across public and private sectors.
- Facility-based IMNCI (F-IMNCI): trains medical officers and staff nurses at First Referral Units (FRUs) for inpatient management of major causes of neonatal and childhood mortality (asphyxia, sepsis, low birth weight, pneumonia, diarrhea, malaria, meningitis, severe malnutrition).
- Master trainers at state/district level are often paediatricians from tertiary hospitals and medical colleges.
Call to action
If you're a health worker, trainer or policymaker: display the wall charts, include neonatal modules in training, and ensure facility readiness. For educators: consider adding IMNCI modules to pre-service curricula and sharing these charts widely within clinical teaching settings.
Further reading / authoritative sources: WHO and UNICEF materials on IMCI/IMNCI, and national program documents (link these from your site's resources or a References block).
If you want, I can also:
- Generate a concise meta description and social share text for Facebook/Twitter/WhatsApp.
- Produce a short infographic-friendly text snippet for a featured image overlay.
- Create a Drupal-friendly "References" list with external links ready to place in the References section or a sidebar (I will format them to meet filtered-HTML rules).
• The most common causes of infant and child mortality in developing countries (including India) are:
– Acute respiratory infections
– Diarrhoea
– Malaria
– Measles and
– Malnutrition
• Making a single diagnosis may not be feasible or appropriate
– Because many children present with overlapping signs and symptoms of diseases
– Clinical outcome depends upon treating not only the immediate presenting symptom but the underlying disorders as well
– This is especially true for first-level health facilities where examinations involve few instruments, little or no laboratory tests, and no X-ray
• Every day, millions of parents seek health care for their sick children, taking them to
– health centers,
– pharmacists,
– doctors
– Hospitals and
– traditional healers
• Surveys reveal that many sick children are
– not properly assessed and treated by these health care providers, and
– That their parents are poorly advised.
• At first-level health facilities in low-income countries, diagnostic supports such as radiology and laboratory services are minimal or non-existent, and drugs and equipment are also scarce.
• These factors make providing quality care to sick children a serious challenge.
• Responding to this challenge, WHO, in collaboration with UNICEF and other agencies, developed a strategy known as the Integrated Management of Childhood Illness (IMCI) *Note that there is no N (neonatal)
The Indian Version – IMNCI (Integrated Management of Neonatal and Childhood Illness)
• This strategy has been adapted for India as Integrated Management of Neonatal and Childhood Illness (IMNCI) because:
– Neonatal mortality contributes to over 64% of infant deaths and most of these deaths occur during first week of life (first week of life was not included in IMCI)
– Mortality rate in the second month of life is also higher than at later ages (training for 7d - 2 month age was given lesser amount of time than that for the age group 2month – 5 yr. )
– Any health program that aims at reducing IMR needs to address mortality in the first two months of life, particularly in the first week of life.
• The IMNCI clinical guidelines target children less than 5 years old — the age group that bears the highest burden of deaths from common childhood diseases.
How is IMNCI Different from IMCI?
• The major highlights of the Indian adaptation are:
– Inclusion of 0 – 7 days age in the program
– Training of the health personnel begins with sick young infants up to 2 months (sick young infant)
• (in IMCI, this is done AFTER the training for 2month – 5 yr.)
– Proportion of training time devoted to sick young infant (0d – 2months age) and sick child (2months – 5 yr. of age) is almost equal
– Is skill based
– Incorporates the national guidelines on
• malaria,
• anaemia,
• vitamin A supplementation and
• immunization schedule
Basis of IMNCI Guidelines
• The IMNCI clinical guidelines target children less than 5 years old — the age group that bears the highest burden of deaths from common childhood diseases.
• The approach to case management is:
– evidence-based and
– syndromic
– that supports the rational, effective and affordable use of drugs and diagnostic tools.
• Evidence-based medicine
– Uses the evidence from clinical research and
– Cautions against the use of intuition, unsystematic clinical experience, and untested pathophysiologic reasoning for medical decision-making.
• In situations where laboratory support and clinical resources are limited, the syndromic approach is a more realistic and cost-effective way to manage patients.
– Careful and systematic assessment of common symptoms and well-selected clinical signs provides sufficient information to guide rational and effective actions.
• So the guidelines based on evidence-based syndromic approach are used by the health worker to determine the:
– Health problem(s) the child may have;
– Severity of the child’s condition;
– Actions that can be taken to care for the child (e.g. refer the child immediately, manage with available resources, or manage at home)
The Integrated Case Management Process
• The case management process is presented on a series of charts, which show the sequence of steps and how to perform them.
• The charts describe the following steps:
1. Assess the young infant or child
• Means taking a history and doing a physical examination.
2. Classify the illness
• “Classify the Illness” means making a decision on the severity of the illness and
• Assigning to a Colour, or “Classification,” which corresponds to the severity of the disease
• Classifications are not specific disease diagnoses. Instead, they are colour coded categories that are used to determine treatment
3. Identify treatment
• The charts recommend appropriate treatment for each colour coded classification
4. Treat the infant or child
• “Treat” means giving treatment in clinic,
• prescribing drugs or other treatments to be given at home, and
• also teaching the mother how to carry out the treatments.
5. Counsel the mother
• assessing how the child is fed and
• telling her about the foods and fluids to give the child and
• when to bring the child back to the clinic.
6. Give follow-up care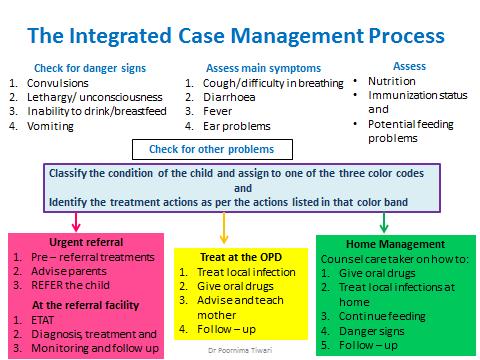
IMNCI Wall Charts
• The case management process is presented on two different sets of charts:
– These charts are to be displayed prominently
1. Management of the young infant age up to 2 months is presented on two charts titled:
a. ASSESS AND CLASSIFY THE SICK YOUNG INFANT AGE UP TO 2 MONTHS and
b. TREAT THE YOUNG INFANT AND COUNSEL THE MOTHER.
2. The case management process for sick children age 2 months up to 5 years is somewhat different from young infants and is presented on three charts titled:
a. ASSESS AND CLASSIFY THE SICK CHILD AGE 2 MONTHS UP TO 5 YEARS
b. TREAT THE CHILD
c. COUNSEL THE MOTHER
• The charts are designed to help you to manage young infants and children correctly and efficiently.
The 3 Components of the IMNCI Strategy
• The strategy actually includes three main components:
1. Improvements in the case-management skills of health staff through the guidelines on Integrated Management of Neonatal and Childhood illness
• This has been discussed above
2. Improvements in the overall health system required for effective management of childhood illness;
3. Improvements in family and community health care practices and involving them in health care process
In addition to these guidelines meant for peripheral health workers, Guidelines for training at other levels have also been developed:
• Pre- service IMNCI
– It is being included in the curriculum of medical colleges of the country.
– This will help in providing the much needed trained IMNCI manpower in the public and private sector.
• Facility based IMNCI (F – IMNCI)
– The F-IMNCI training would provide the optimum skills needed by the Medical officers and Staff Nurses at the FRU’s (First Referral Unit)
– Thereby helps to address the acute shortage of Pediatricians at facilities
– It focusses on providing appropriate inpatient management of the major causes of neonatal and childhood mortality such as asphyxia, sepsis, low birth weight, pneumonia, diarrhea, malaria, meningitis and severe malnutrition in children at the FRU
– The master trainers at state and district level are pediatricians from tertiary hospitals and medical colleges.
References:
• Park’s Textbook of Preventive and Social Medicine
• Ministry of Health & Family Welfare Government of India New Delhi 2009; INTEGRATED MANAGEMENT OF NEONATAL AND CHILDHOOD ILLNESS (IMNCI) Modules 1 to 9
• Integrated Management of Childhood Illness (IMCI), WHO website: Available at: http://www.who.int/maternal_child_adolescent/topics/child/imci/en/ accessed on 5th August 2017
• Ministry of Health & Family Welfare Government of India New Delhi 2009; Facility Based (F-IMNCI) Participants Manual
5-Page ANC History Taking Format: https://ihatepsm.com/blog/5-page-anc-history-taking-format-essential-gui...
Why ANC History Taking Matters?: https://ihatepsm.com/blog/why-anc-history-taking-matters
Taking a Meaningful Clinical History: https://ihatepsm.com/blog/taking-meaningful-clinical-history
Format for Clinical History Taking: https://ihatepsm.com/blog/format-clinical-history-taking
History taking in a paediatric patient: https://ihatepsm.com/blog/history-taking-paediatric-patient
Format for CSC taking: http://www.ihatepsm.com/blog/format-clinico-social-case-taking-community...
Geriatric Clinico-Social Case: https://ihatepsm.com/blog/geriatric-clinico-social-case-community-medicine
