Control of Diphtheria
1. Treatment of
– Cases and
– Carriers
– Management of the ‘Contacts’ and
3. At the community level
– Increasing coverage of immunization with diphtheria toxoid
Treatment of Cases and Carriers
Early detection
• An active search for cases and carriers should start immediately amongst family and school contacts
• Carriers can be detected ONLY by culture
• Swabs should be taken from both the nose and throat
• Examined by culture for diphtheria bacilli
• Tests should also be done for virulence of the organism
Isolation
• All cases
• Suspected cases and
• Carriers should be
• Promptly isolated
• Preferably in a hospital
• For at least 14 days or
• Until proved free of infection
• At least 2 consecutive
• nose and throat swabs,
• taken 24 hours apart
• should be negative before terminating isolation
Treatment of cases and carriers
• Cases:
– Diphtheria antitoxin should be given without delay,
• IM or IV, Dose ranges from 20,000 to 1,00.000 units depending up on the severity
• Mild early pharyngeal or laryngeal disease: 20 to 40,000 units
• Moderate nasopharyngeal disease : 40 to 60, 000 units
• For severe, extensive or late (≥3 days): 80 to 1,00,000 units
– Penicillin or erythromycin for 5 – 6 days to clear the throat of C. diphtheriae and thereby decrease toxin production
– The case should be reported to the health authorities Immediately
– Once recovered, active immunization with diphtheria toxoid should be provided
• Carriers:
– Treat with 10 days course of oral erythromycin
Management of Contacts
Contacts merit special attention
1. They should be throat swabbed
2. Determine the immunization status and take further action accordingly (shown below)
3. Contacts need to be placed under medical surveillance
– Examined daily for evidence of diphtheria for one week
– Bacteriological surveillance weekly for several weeks (weekly swabbing)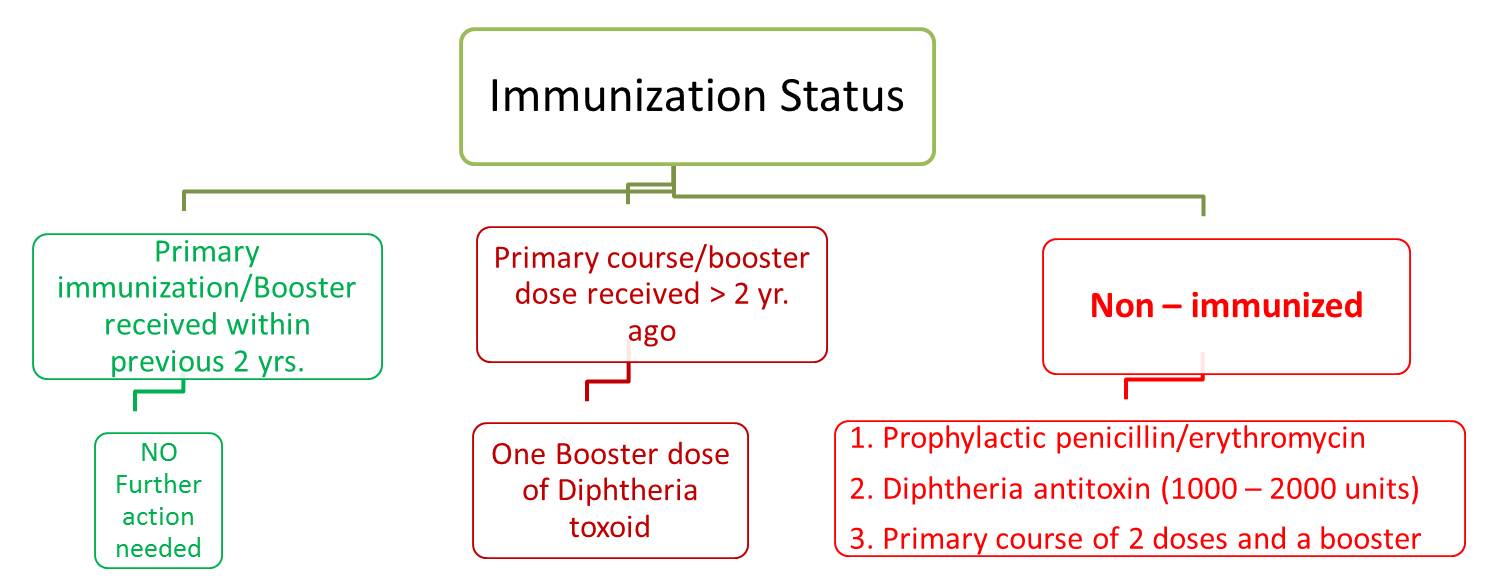
Control in the Community
• The only effective control is by active immunization
– With diphtheria toxoid
– Of all infants
– As early in life as possible
– Subsequent booster doses every 10 years thereafter
• The aim is to immunize before the infant loses the maternally derived immunity
– So that there is continuous protection from birth without any gap in immunity to natural disease
• Immunization does not prevent the carrier state
• As the vaccine being a toxoid is not directed against the organisms
• Hence non immune individuals are not protected by a high level of population coverage
• This implies that immunization must be maintained at high level
Diphtheria Immunization
The toxoid vaccine is available in different forms as mentioned below:-
• Combined/mixed vaccines
– DPT (Diphtheria, Pertussis, Tetanus) vaccine
– Pentavalent vaccine (Diphtheria, Pertussis, Tetanus, Hepatitis B and Hib)
– DTaP (Diphtheria, acellular Pertussis, Tetanus) vaccine
– DT (Diphtheria, Tetanus toxoid) vaccine
– dT (Diphtheria, Tetanus -adult type) vaccine
– DTaP, IPV, HepB (Diphtheria, acellular Pertussis, Tetanus with hepatitis B and Polio)
• Paediatric formulations (DT, DPT and DTaP) contain a similar amount of tetanus toxoid as adult Td, but contain 3-4 times as much diphtheria toxoid.
• Single vaccines
– FT (Formal toxoid)
– APT (Alum precipitated toxoid)
– PTAP (Purified toxoid aluminium phosphate)
– PTAH (Purified toxoid aluminium hydroxide)
Immunization Schedule for Diphtheria
For routine immunization of infants:
• Combined vaccines are preferred
– Simultaneous immunization against more than one disease
– The pertussis component enhances the potency of diphtheria toxoid
• Optimum age: as early as 6 weeks
– Young infants respond well even in presence of low to moderate levels of maternal antibodies
• Number of doses
– Three doses of DPT/ Pentavalent vaccine/ DTaP+ IPV+ HepB
– 4 weeks apart (6, 10, & 14 weeks of age as per NIS)
– for primary immunization
• Booster at least 6 months later and AFTER 12 months of age (16 – 24 months as per National Immunization Schedule or NIS)
– Second booster (DT only) at 5 – 6 yr.
• Dosage – 0.5 ml
• Route of administration – deep intramuscular (IM)
• Site of administration – Lateral aspect of thigh for infants
For older children: After 5 yr of age –
• Only 2 doses of DT,
• 4 weeks apart,
• Booster 6 months – 1 yr, later
For children > 12 yr. old and Adults
• Preparation of choice is dT
This is the adult type of diphtheria tetanus vaccine
It contains much lesser amount of diphtheria toxoid but same amount of TT as pediatric preparation
Antisera
• Diphtheria antitoxin, prepared in horse serum
• Is still the mainstay of passive prophylaxis and treatment of diphtheria
• It has been shown that protection against diphtheria toxin is a quantitative phenomenon
• A serum antitoxin titer against a small dose of toxin may not protect against a larger dose
• Failure of diphtheria immunization may occur due to this phenomenon
References
• DIPHTHERIA - A RE-EMERGING THREAT. CD Alert, Jan – Mar 2008; 12 (1): 1-8 available on http://www.ncdc.gov.in/writereaddata/linkimages/Jan-March%20087398246488... downloaded on 16 Dec 2016
• Communicable Disease Management Protocol – Diphtheria. August 2016. available at: http://www.gov.mb.ca/health/publichealth/cdc/protocol/diphtheria.pdf downloaded on 16 Dec 2016
• http://www.immunize.org/catg.d/p4203.pdf accessed on 16 Dec 2016
• Park’s Textbook of Preventive and Social Medicine, 23rd Edition, Diphtheria, 161-163
Control of diphtheria: http://www.ihatepsm.com/blog/control-diphtheria
Management of Contacts of a Case of Diphtheria: http://www.ihatepsm.com/blog/management-contacts-diphtheria-case
Diphtheria – Epidemiology, Clinical Features & Management: http://www.ihatepsm.com/blog/diphtheria-%E2%80%93-epidemiology-clinical-...
